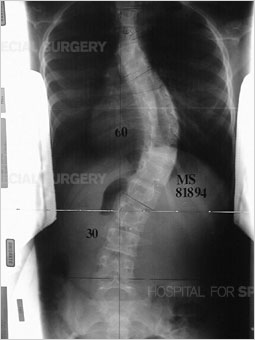
Before I describe what it was like after surgery, here are my x-rays before the operation.
My three curves were measured 34 degrees, 54 degrees, and 28 degrees, from top to bottom. Because that 54 is clearly above the 45-50 degree operative level, that meant I needed surgery. However, because I also had a chiari malformation (when the brain tissue extends into the spinal canal) I needed another surgery. I talked about this in an earlier post, how the brain tissue can cause syrinx (pockets of spinal fluid) to build up in the spine, and that can be dangerous for spinal fusion patients.
In my last post I talked about before the surgery, but now I'll talk about what happens after.
Most people stay in the ICU for one day, although Dr.Shindell is working to find a way to make that not necessary, where they're under high surveillance. Within the first day following the surgery, the doctors have the patient start walking, though with some assistance. I, on the other hand, had to stay in the ICU for two days, as I had a severe drop in blood pressure, causing me to go blue, and causing my parents to have to wait to see me for a few extra hours after.
I wish I could say that I remembered the hospital visit, but I don't, not one bit of it, so here's what my dad said about what I was like,
"You were very antsy, and wanted to be moved around every five minutes, most likely because your body was getting used to being at a different angle. You kept asking to be adjusted. We didn't know if your body was producing cortisol (the hormone they thought was causing your drop in blood pressure). You were very emotional, you wanted to make sure you weren't being a burden. You walked as fast as possible when they asked you to walk because you hated it."
Following about 6 days in the hospital, I was sent home, with a walker, and pain medication (which I didn't take much of after a little while).
For about three weeks, I was in bed, and occasionally following that time, I would leave my bedroom and start walking with the walker, only to sit in the living room chair instead, just for meals.
I didn't eat much, and lost about 11 pounds following the surgery.
Because they thought my body wasn't producing cortisol, they put me on a medication to try and boost the levels of that hormone, and even sent me around with a needle and liquid medication just in case I passed out.
I wasn't allowed to carry anything over 10lbs, and I very often got tired. My muscles ached more than anything, as they cut through a lot of muscle to get down to your spine. Even to this day, over 3 months since the surgery, I still get severe muscle pain in my shoulders when I do too much.
There's so much more that I experienced after the surgery that I either don't remember, or don't want to overwhelm you with, but I feel that these past two blog posts have been pretty informative.
Here is my spine now.
The curve is 28 degrees, which is very good, as very few surgeries actually get full fusion.
The reason I'm trying to study the complications now, is because I had a preoperative condition, and I had postoperative complications (the very low blood pressure) and I wanted to know if they are connected.
I still struggle with data, but with the small amount that I have plus some readings I found, I should be able to get some understanding, but of course this is just a high school project and not an actual government funded research.
Are complications following spinal fusion surgery for pediatric scoliosis related to other pre-surgical physical disorders or diseases? Are there preventative measures that doctors can take to lower the incidence of postoperative complications?
Tuesday, March 28, 2017
Saturday, March 25, 2017
Week Seven Day Two: In the Eyes of a Patient (pt 1).
Because my project is very personal to me, and something I've dealt with, I thought I'd go ahead and share how this surgery works from the patient's perspective, starting from the night before/morning of the surgery. This might get long, considering I have a lot to say, but that's why I'm splitting it into two parts.
Two days before the surgery, I went to the hospital to do blood work. While I was there, a pediatric child life specialist came in and gave me a small run down of what would happen the morning of the surgery, such as that I will meet with my surgeon, and my anesthesiologist, as well as showing me pictures of the OR. They put it in very child like terms, as I was staying in a children's hospital to get this done. They also gave me these wipes (which I had used before my other surgery) that you're supposed to put on the night before surgery, after you've showered and dried, and the morning of surgery, where you're not supposed to shower.
I had to stop eating at midnight, so because I am very dramatic and told myself I would starve the next morning, I literally made mac and cheese around 11:30 so I could eat right until the end.
Sleeping was hard, as I was stressed and nervous. I had to leave the house at 5:30am to get there, as my surgery was scheduled for 7am and I had to get there an hour early for checkin and getting an IV placed in my arm so they could put me under.
I got dressed in the worst clothes I had, grabbed my blanket, and sat in the back of my mom's car as she drove me there. They gave me permission to bring a comfort item back to surgery, as well as a camera, so I brought my blanket.
In the pre-op room, they gave me a gown to put on, and they told me to get completely undressed, then get onto the bed. There's a whole room to yourself, and my parents and I watched Zootopia, and talked about my nephew.
I was freezing, even under the few blankets they gave me, and I was shaking, out of fear as well as the cold. A nurse came in and put my IV in my arm, but made sure to give me a numbing medication beforehand so I wouldn't feel the needle go in. We waited for a while, and met with the anesthesiologist, and made sure to explain to them that I get sick after anesthetics, so they would add a medication in it to make sure I didn't. Then I met with my surgeon, and he told me what was going to happen, even though we've already gone over it plenty of times.
After all that, a few more minutes passed before a nurse came in and told my parents it was time to take me back. I kissed them both goodbye, and my nurse wheeled me down the hall into the OR. I know we talked about something, possibly school, but I can't quite remember. When we got to the OR I saw everything, the table, the bright lights, literally everything.
The nurse told me she was going to give me the first part of the anesthetics, and then told me to count down from ten. After that, I can't remember much.
I'll explain in the next post, the second half of the surgery, aka recovery, but I thought it'd be interesting to put in my own perspective of the two days beforehand, and the morning of.
Two days before the surgery, I went to the hospital to do blood work. While I was there, a pediatric child life specialist came in and gave me a small run down of what would happen the morning of the surgery, such as that I will meet with my surgeon, and my anesthesiologist, as well as showing me pictures of the OR. They put it in very child like terms, as I was staying in a children's hospital to get this done. They also gave me these wipes (which I had used before my other surgery) that you're supposed to put on the night before surgery, after you've showered and dried, and the morning of surgery, where you're not supposed to shower.
I had to stop eating at midnight, so because I am very dramatic and told myself I would starve the next morning, I literally made mac and cheese around 11:30 so I could eat right until the end.
Sleeping was hard, as I was stressed and nervous. I had to leave the house at 5:30am to get there, as my surgery was scheduled for 7am and I had to get there an hour early for checkin and getting an IV placed in my arm so they could put me under.
I got dressed in the worst clothes I had, grabbed my blanket, and sat in the back of my mom's car as she drove me there. They gave me permission to bring a comfort item back to surgery, as well as a camera, so I brought my blanket.
In the pre-op room, they gave me a gown to put on, and they told me to get completely undressed, then get onto the bed. There's a whole room to yourself, and my parents and I watched Zootopia, and talked about my nephew.
I was freezing, even under the few blankets they gave me, and I was shaking, out of fear as well as the cold. A nurse came in and put my IV in my arm, but made sure to give me a numbing medication beforehand so I wouldn't feel the needle go in. We waited for a while, and met with the anesthesiologist, and made sure to explain to them that I get sick after anesthetics, so they would add a medication in it to make sure I didn't. Then I met with my surgeon, and he told me what was going to happen, even though we've already gone over it plenty of times.
After all that, a few more minutes passed before a nurse came in and told my parents it was time to take me back. I kissed them both goodbye, and my nurse wheeled me down the hall into the OR. I know we talked about something, possibly school, but I can't quite remember. When we got to the OR I saw everything, the table, the bright lights, literally everything.
The nurse told me she was going to give me the first part of the anesthetics, and then told me to count down from ten. After that, I can't remember much.
I'll explain in the next post, the second half of the surgery, aka recovery, but I thought it'd be interesting to put in my own perspective of the two days beforehand, and the morning of.
Wednesday, March 22, 2017
Week Seven Day One: The Issue with Genetics.
After talking to Doctor Shindell yesterday, and knowing that he has said, not only to me, but to all his patients that scoliosis is a genetic issue, I now know that the main question is: how? There is no certain answer as to what gene directly causes scoliosis, although plenty of research has been done on the subject.
When parents or grandparents have a known history of scoliosis, it's common for them to watch out for their children to see if/when the scoliosis takes an obvious form.
According to this website (The National Library of Medicine) there are different genetic and environmental factors that contribute to a child having scoliosis, however, when a "close relative" has idiopathic scoliosis, it increases a child's risk at having the disorder as well.
Although I didn't have access to the full text, in an abstract for an article called "Genetics of Scoliosis" by Robert F Henry ,M.D., and Karthik Madhavan, M.D., it is proposed that the gene for scoliosis is either autosomal dominant, X-linked, multigene, or multifactoral. None of these have actually been proven true and are still just theories.
Although knowing the gene isn't a pressing issue that needs to be figured out, it is still largely important as some theorize that the genetics of the disorder can also call for how severe the curve is and can be the difference between 20 degrees (top) and 60 degrees (bottom) which is also the difference between bracing and operation.
Of course, if (hypothetically) science gets to the point where doctors can calculate the projected amount of curvature, the doctor would and should still brace as the "projected amount" could be avoidable.
However this begs the question, is putting money into this research really a large need? But that's another issue on its own.
When parents or grandparents have a known history of scoliosis, it's common for them to watch out for their children to see if/when the scoliosis takes an obvious form.
According to this website (The National Library of Medicine) there are different genetic and environmental factors that contribute to a child having scoliosis, however, when a "close relative" has idiopathic scoliosis, it increases a child's risk at having the disorder as well.
Although I didn't have access to the full text, in an abstract for an article called "Genetics of Scoliosis" by Robert F Henry ,M.D., and Karthik Madhavan, M.D., it is proposed that the gene for scoliosis is either autosomal dominant, X-linked, multigene, or multifactoral. None of these have actually been proven true and are still just theories.
Although knowing the gene isn't a pressing issue that needs to be figured out, it is still largely important as some theorize that the genetics of the disorder can also call for how severe the curve is and can be the difference between 20 degrees (top) and 60 degrees (bottom) which is also the difference between bracing and operation.
Of course, if (hypothetically) science gets to the point where doctors can calculate the projected amount of curvature, the doctor would and should still brace as the "projected amount" could be avoidable.
However this begs the question, is putting money into this research really a large need? But that's another issue on its own.
Saturday, March 18, 2017
Week Six Day Two: Collecting Data and Fun Facts.
So, yesterday at the office, it was a busy and hectic day. The doctor was on call, and definitely got a lot of calls, for emergencies at Phoenix Children's Hospital. At least for me it was enlightening on what it was like to be a surgeon on call. Hectic, the only word I can really think of to describe it. Dr.Shindell even apologized to me for it being so hectic.
Anyways, moving on from that story to the stuff I know you're all dying to know. How am I going to collect enough data to support an argument. Well... at first I didn't know. I was convinced I could do some data mining at the office, but that didn't prove true, so I contacted a scoliosis association called "Curvy Girls" that one of the parents recommended to me when they found out that I had scoliosis surgery myself. They have an online board for people to talk about their scoliosis and everything related to it, so I decided to reach out to them and see if there was anyway I could send out a survey for people who had the spinal fusion surgery. Currently it's waiting review, but I'm going to try and contact them again tomorrow about it. The only thing that concerns me is that this might come together at the last minute, but I'm doing my best to try and get as much data as possible.
I know that talking about data may be boring so I decided to spice up this post with some celebrities that have scoliosis.
Sarah Michelle Gellar - You probably know her as Buffy from Buffy the Vampire Slayer TV show.
Shailene Woodley- Known for her role as Tris Prior in the Divergent Series Movies.
Laura Dern- I know her for her role in Jurassic Park but she's been in much more.
Many more celebrities have scoliosis, considering 2-3% of the population has scoliosis, this isn't really shocking. I hope this has been fun and informative, and please expect more in detail posts next week.
Anyways, moving on from that story to the stuff I know you're all dying to know. How am I going to collect enough data to support an argument. Well... at first I didn't know. I was convinced I could do some data mining at the office, but that didn't prove true, so I contacted a scoliosis association called "Curvy Girls" that one of the parents recommended to me when they found out that I had scoliosis surgery myself. They have an online board for people to talk about their scoliosis and everything related to it, so I decided to reach out to them and see if there was anyway I could send out a survey for people who had the spinal fusion surgery. Currently it's waiting review, but I'm going to try and contact them again tomorrow about it. The only thing that concerns me is that this might come together at the last minute, but I'm doing my best to try and get as much data as possible.
I know that talking about data may be boring so I decided to spice up this post with some celebrities that have scoliosis.
Sarah Michelle Gellar - You probably know her as Buffy from Buffy the Vampire Slayer TV show.
Shailene Woodley- Known for her role as Tris Prior in the Divergent Series Movies.
Laura Dern- I know her for her role in Jurassic Park but she's been in much more.
Many more celebrities have scoliosis, considering 2-3% of the population has scoliosis, this isn't really shocking. I hope this has been fun and informative, and please expect more in detail posts next week.
Tuesday, March 14, 2017
Week Six Day One: The Older Days.
Cast after cast after cast in the first thirty minutes today, apparently children get hurt often on the playground, who ever would've guessed? Anyways, that's besides the point. Today was a shorter day for patient visits, but I was able to read some interesting things in the book, Scoliosis: Ascending The Curve, about how scoliosis surgery was about fifty years ago.
First of all, I read that instrumentation wasn't even used, it didn't go in depth on how this surgery would've worked without instrumentation, but this is all for my own pleasure in trying to understand how lucky other recent patients and I have been with the evolution of treatment that has happened over this time period with shortened hospital stays, better/more available instrumentation, and not having the large preoperative examination that used to be standard.
In this examination, patients had to stand in a swimsuit in front of 20 or so doctors for them to look at the patient and see them visually before taken back for surgery.
They also had to go through a series of full body casts for six weeks, to prepare her for the traction she would have to go through for those six weeks before the surgery. People used to call it the "torture chamber" according to this book.
Because there instrumentation was new and rarely used, when it wasn't used, the spine was straightened by force and a bone graft.
We've come a long way from there and now make it easier on patients to recover, with most of them able to walk the day after surgery rather than the two months after that most people used to have to do because of full body casts.
First of all, I read that instrumentation wasn't even used, it didn't go in depth on how this surgery would've worked without instrumentation, but this is all for my own pleasure in trying to understand how lucky other recent patients and I have been with the evolution of treatment that has happened over this time period with shortened hospital stays, better/more available instrumentation, and not having the large preoperative examination that used to be standard.
In this examination, patients had to stand in a swimsuit in front of 20 or so doctors for them to look at the patient and see them visually before taken back for surgery.
They also had to go through a series of full body casts for six weeks, to prepare her for the traction she would have to go through for those six weeks before the surgery. People used to call it the "torture chamber" according to this book.
Because there instrumentation was new and rarely used, when it wasn't used, the spine was straightened by force and a bone graft.
We've come a long way from there and now make it easier on patients to recover, with most of them able to walk the day after surgery rather than the two months after that most people used to have to do because of full body casts.
Friday, March 10, 2017
Week Five Day Two: A Misunderstanding and Change in Data
Well, this project is meant to be educational, and a learning experience, which therefore means there will be some mistakes and misunderstandings. This post may be short, but this was kind of the focus of today (other than my internship site getting me dairy queen, which was a nice end to my week).
A few blog posts ago, maybe the second to last one, I talked about MAGEC rods and how they related to spinal fusion, however due to a small misunderstanding on my behalf, the surgery those children have who are still in the process of growing is not considered spinal fusion.
In the regular spinal fusion surgery, whether done anteriorly or posteriorly the spine is legitimately fused together, however, and this should make sense by using any sort of common sense children who are still growing should not have their spine fused, as it could lead to issues with their height and health, and back pain, and so on.
This to me really just shows one thing, that I'm going to struggle more than I thought I would with collecting data. I can try to data mine, or possibly ask for some data points from Dr. Shindell himself, or even use data collected through other studies, to put together a well rounded set of data to answer my question, but I still fear a significant lack in this data.
From the beginning of the project, I knew the amount of data would be my number one problem with this project (that, as well as my emotional connection to the project, which I will explain in another post), but at the end of the day, this is a great learning and personal experience that I'm very grateful for, and I will try my best to try and collect enough data to have some sort of analysis. Some people say 6 is a minimum, while others say 10, which is what I'm hoping for. I'll keep everyone updated with how the data collection is going throughout my other blog posts during this project.
A few blog posts ago, maybe the second to last one, I talked about MAGEC rods and how they related to spinal fusion, however due to a small misunderstanding on my behalf, the surgery those children have who are still in the process of growing is not considered spinal fusion.
In the regular spinal fusion surgery, whether done anteriorly or posteriorly the spine is legitimately fused together, however, and this should make sense by using any sort of common sense children who are still growing should not have their spine fused, as it could lead to issues with their height and health, and back pain, and so on.
This to me really just shows one thing, that I'm going to struggle more than I thought I would with collecting data. I can try to data mine, or possibly ask for some data points from Dr. Shindell himself, or even use data collected through other studies, to put together a well rounded set of data to answer my question, but I still fear a significant lack in this data.
From the beginning of the project, I knew the amount of data would be my number one problem with this project (that, as well as my emotional connection to the project, which I will explain in another post), but at the end of the day, this is a great learning and personal experience that I'm very grateful for, and I will try my best to try and collect enough data to have some sort of analysis. Some people say 6 is a minimum, while others say 10, which is what I'm hoping for. I'll keep everyone updated with how the data collection is going throughout my other blog posts during this project.
Wednesday, March 8, 2017
Week Five Day One: What Defines a Complication?
Today in the office, we sadly had no patients who had the spinal fusion surgery that I have been studying, but that didn't stop me from trying to think of ways to improve my project and my data collection. The term complication is very broad, and (when using google) is described as:
A circumstance that complicates something; a difficulty
This by no means isn't true, but does not fit my project or give me any basis of trying to decided whether or not something that happened following spinal fusion is a complication or not. So, for my project, I describe it as:
An unexpected result of spinal fusion surgery
This has worked for the patients I have seen so far, but through data mining from reliable medical publications, I have realized that there can be some "unexpected results" that actually are not harmful (which was what I originally had in mind for this project) such as the degree of curvature decreasing past the expected amount, or a patient growing more than the doctor had expected.
This has led me to have to try and mold the definition around to try and make my project and research more clear. Now I have formed the definition to be:
An unexpected and unwanted result of spinal fusion surgery.
This rules out the sort of "positive" and unexpected results of the surgery.
That data I have collected so far says that out of the kids who had preoperative conditions, 2/4 of them had complications. The data so far is small, but I plan to talk to Dr. Shindell about some patients with complications that he knows, as well as using some data mining from outside resources.
Friday, March 3, 2017
Week Four Day Two: MAGEC Rods
A few days ago, I was able to learn about scoliosis in infants and pre pubescent children. Normally, pre pubescent children who have scoliosis can be treated with a brace if the degree of curvature passes 20 degrees. This brace would try to restrict the curve from increasing at the child grew and developed. However, there are some cases where kids have the 45+ degrees and are still growing. In this case, surgery is the best option to try and reduce the curve.
Once a child has reached puberty, and is fully grown, the curve is less likely to increase. Take these two cases for example.
1 ) A 16 year old female, who is fully grown, with a 30 degree curve.
2 ) A 9 year old female, who still has lots to grow, with a 30 degree curve.
In case one, it'd be most likely that the orthopedic specialist wouldn't do anything for the curve, other than checking it out again six months to a year later, to ensure it isn't growing. There would be no bracing, and no surgery.
In case two, the girl would most likely be put in a brace to stop the increase of the curve. If there is no brace, she would be at high risk for the curve to increase into what I like to call the red zone, which is 45+ degrees, implying possible or guaranteed surgery.
So, picture a 6 year old with a 50 degree curve (below is a picture of a 50 degree curve in an adult for reference).
This child would be at extremely dangerous chance of increasing their curve as they grew, and since the curve is 50 degrees, it would be in the surgical point of development.
However, it is impossible and highly dangerous to put rods and screws in a child who is growing and developing (that should be quite obvious). Because of that, there are rods called MAGEC Rods.
The rods can be placed in growing children for their surgery, and can actually be lengthened while still in the child's body. It's an extremely strange concept, especially when you see in person how the rods are lengthened.
In this picture, if you look closely on the rods, there is one location on each rod that seems a bit darker grey, with a white line in the middle. That is where the rods are lengthened. I was able to see three lengthenings while doing my shadowing experience. It is done by placing a magnetic tool on the child's back to stretch the metal rods out while in the child. No extra incision is needed, and it can be done simply at a specialist's office with the correct tools.
The three instances I saw all helped with the data I was collecting, as all of the instances included pre-existing conditions before the operation, and gave me three more data points in that one day. As someone who had scoliosis, and the surgery, this was a very humbling experience, as I saw kids younger than me having to go through what was the roughest period of my life so far. I'm overall grateful for what I saw, as it gave me a lot of perspective. I cannot wait to continue this experience and hope to learn more about my own condition through observation.
Once a child has reached puberty, and is fully grown, the curve is less likely to increase. Take these two cases for example.
1 ) A 16 year old female, who is fully grown, with a 30 degree curve.
2 ) A 9 year old female, who still has lots to grow, with a 30 degree curve.
In case one, it'd be most likely that the orthopedic specialist wouldn't do anything for the curve, other than checking it out again six months to a year later, to ensure it isn't growing. There would be no bracing, and no surgery.
In case two, the girl would most likely be put in a brace to stop the increase of the curve. If there is no brace, she would be at high risk for the curve to increase into what I like to call the red zone, which is 45+ degrees, implying possible or guaranteed surgery.
So, picture a 6 year old with a 50 degree curve (below is a picture of a 50 degree curve in an adult for reference).
This child would be at extremely dangerous chance of increasing their curve as they grew, and since the curve is 50 degrees, it would be in the surgical point of development.
However, it is impossible and highly dangerous to put rods and screws in a child who is growing and developing (that should be quite obvious). Because of that, there are rods called MAGEC Rods.
The rods can be placed in growing children for their surgery, and can actually be lengthened while still in the child's body. It's an extremely strange concept, especially when you see in person how the rods are lengthened.
In this picture, if you look closely on the rods, there is one location on each rod that seems a bit darker grey, with a white line in the middle. That is where the rods are lengthened. I was able to see three lengthenings while doing my shadowing experience. It is done by placing a magnetic tool on the child's back to stretch the metal rods out while in the child. No extra incision is needed, and it can be done simply at a specialist's office with the correct tools.
The three instances I saw all helped with the data I was collecting, as all of the instances included pre-existing conditions before the operation, and gave me three more data points in that one day. As someone who had scoliosis, and the surgery, this was a very humbling experience, as I saw kids younger than me having to go through what was the roughest period of my life so far. I'm overall grateful for what I saw, as it gave me a lot of perspective. I cannot wait to continue this experience and hope to learn more about my own condition through observation.
Subscribe to:
Posts (Atom)